代謝症候群五大指標,你中了幾項?
小心!罹患糖尿病風險高6倍
作者|初日診所 許芷瑜醫師
「代謝症候群」是現代人的常見健康問題,常伴有高血糖、高血壓、高膽固醇等症狀,增加罹患心血管疾病和糖尿病的風險。初日診所-許芷瑜 醫師將在本文中,為我們詳細解釋代謝症候群的診斷標準、風險因子及預防措施。
代謝症候群是什麼?
代謝症候群是一組綜合症狀,包括高血糖、高血壓、高血脂和腹部肥胖。它不是單一疾病,但若不及時處理,會大大增加糖尿病、心臟病和中風的風險。在台灣,代謝症候群的盛行率高達24.8%,相當於每四個成年人中就有一人受影響。
 代謝症候群的元兇竟是「胰島素阻抗」!
代謝症候群的元兇竟是「胰島素阻抗」!
代謝症候群的診斷標準
要診斷代謝症候群,需要滿足以下五個標準中的至少三項:
腹部肥胖:
男性腰圍≥90cm,女性腰圍≥80cm。
血壓偏高:
收縮壓≥130mmHg或舒張壓≥85mmHg。
空腹血糖偏高:
空腹血糖值≥100mg/dL。
空腹三酸甘油酯偏高:
≥150mg/dL。
高密度脂蛋白膽固醇偏低:
男性<40mg/dL,女性<50mg/dL。
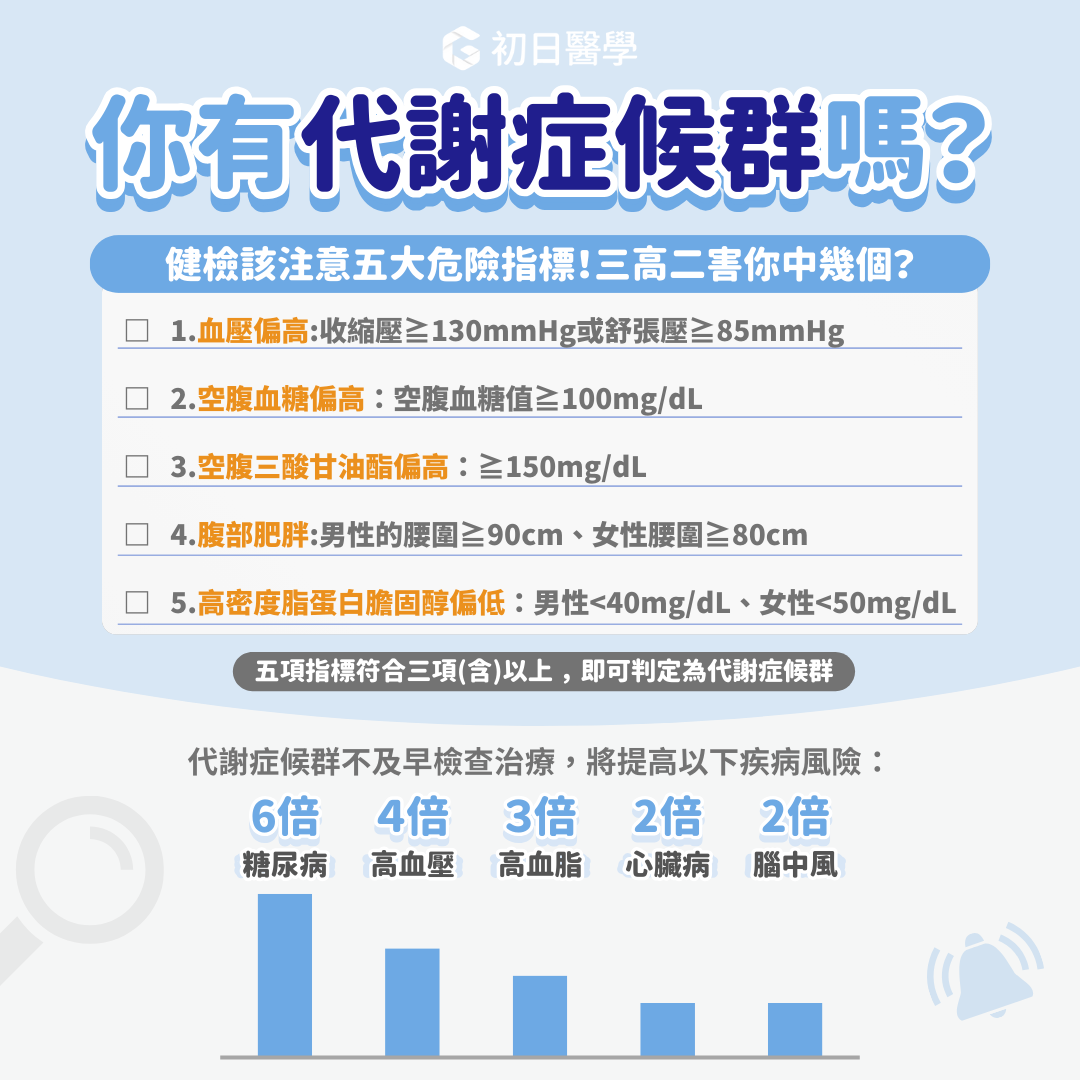 三高+二害,你有代謝症候群嗎?若不治療,恐增加「這些」疾病風險!
三高+二害,你有代謝症候群嗎?若不治療,恐增加「這些」疾病風險!
代謝症候群6大危險因子
1. 遺傳因素:
家族中有高血壓、糖尿病或高血脂病史的人,罹患代謝症候群的風險較高。
2. 缺乏運動:
運動不足不僅會導致肥胖,還會增加心血管疾病和第二型糖尿病的風險。
3. 不良飲食習慣:
超加工食品:含有大量反式脂肪和ω-6脂肪酸,會增加體內發炎因子,導致慢性發炎。
精緻澱粉:過量攝取精緻澱粉會導致體重增加,增加代謝症候群風險。
4. 抽菸:
吸菸會增加腰圍、三酸甘油酯和降低高密度脂蛋白膽固醇,從而增加代謝症候群風險。
5. 飲酒:
重度飲酒會提高罹患代謝症候群的風險,酒精會損害腸道和肝臟功能,導致全身性發炎。
6. 壓力:
長期壓力會引起慢性發炎,進而提高代謝異常的風險。
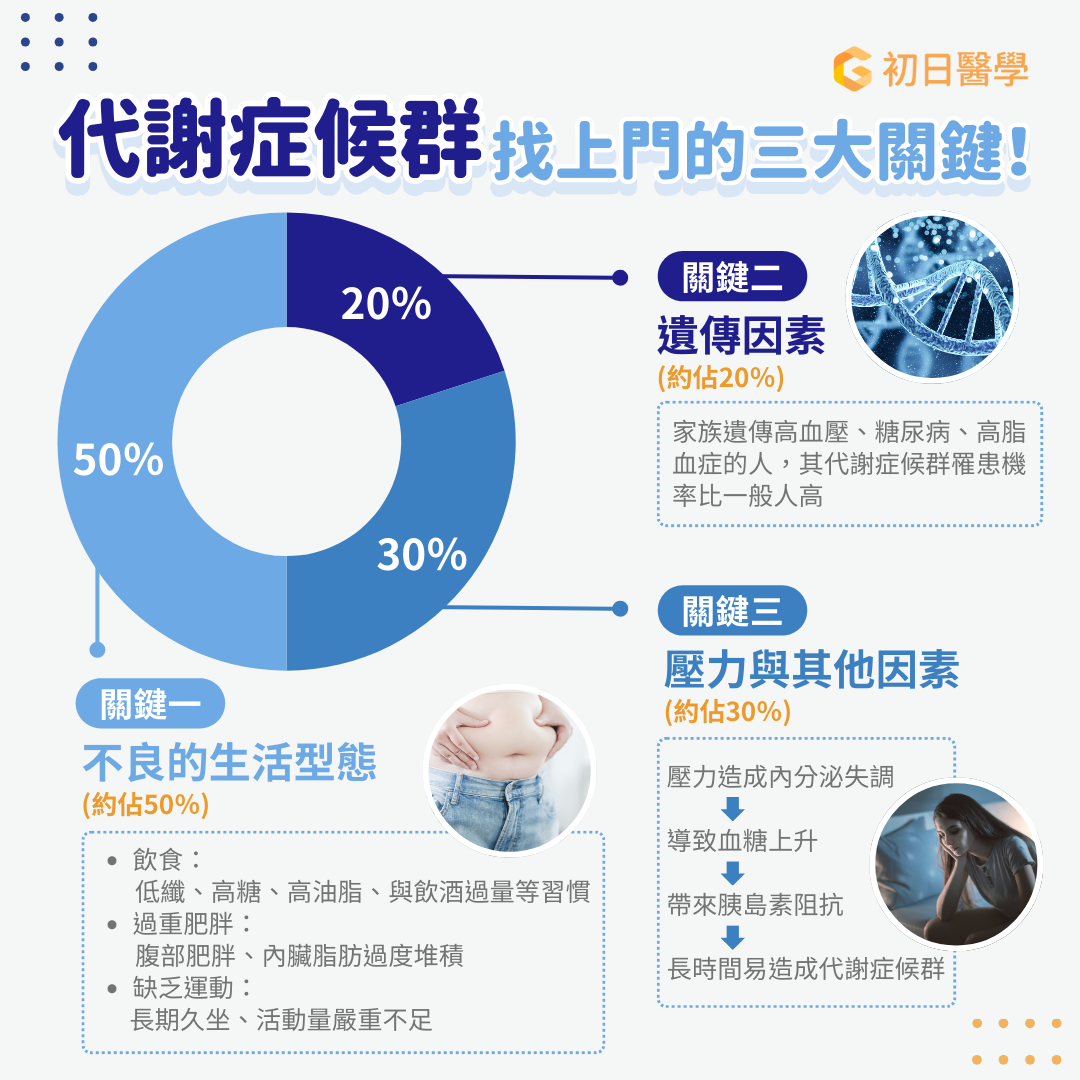 哪些人比較容易得到代謝症候群?三大關鍵因素要注意!
哪些人比較容易得到代謝症候群?三大關鍵因素要注意!
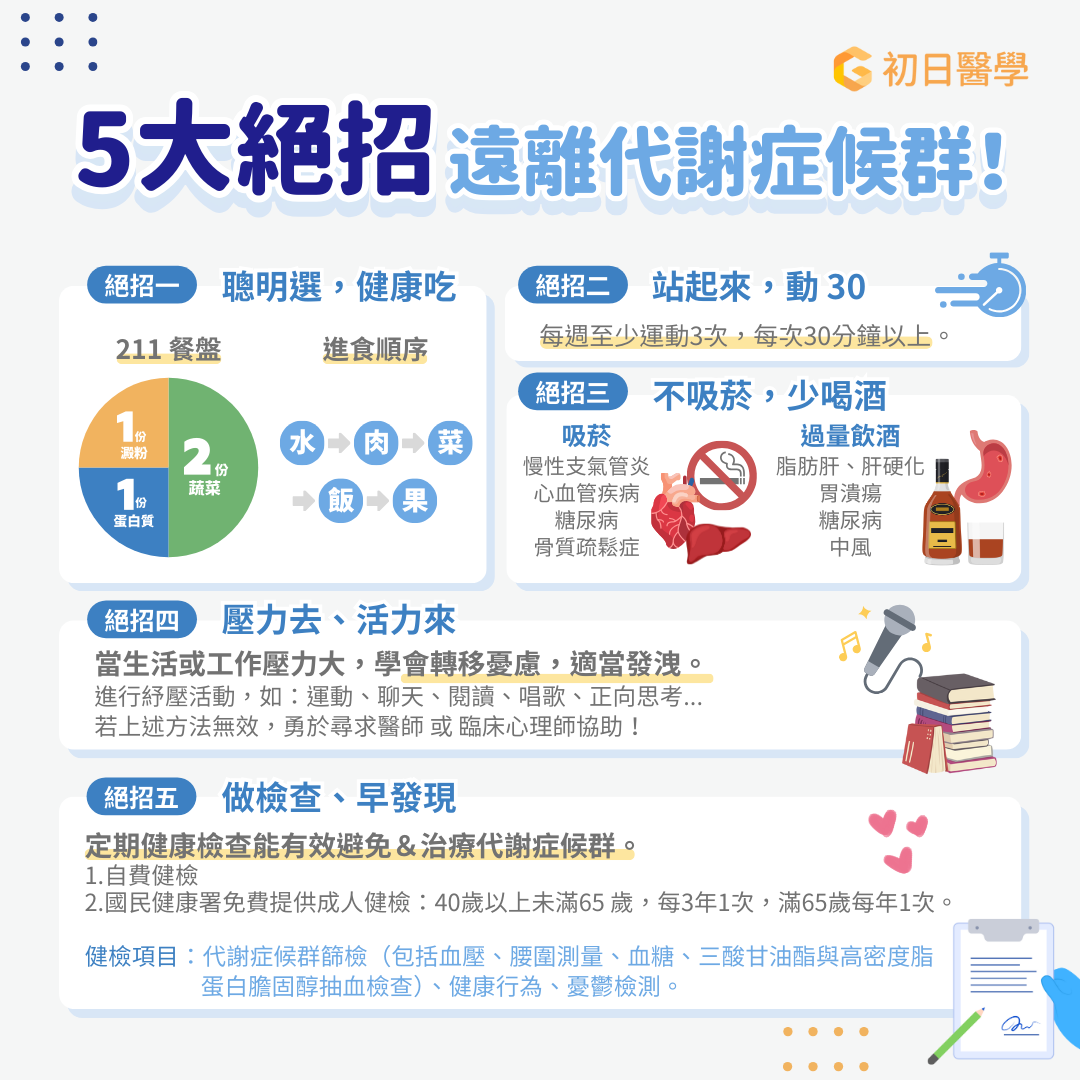
如何預防代謝症候群?
國民健康署提供了五個實用建議:
1. 聰明選,健康吃:
遵循211飲食原則,多吃蔬菜,選擇優質蛋白質和油脂。
2. 站起來,動30:
每天至少運動30分鐘,即使在辦公室久坐,也要多爬樓梯、多走路。
3. 不吸菸,少喝酒:
戒菸和控制飲酒,避免代謝疾病的風險。
4. 壓力去、活力來:
適當釋放壓力,避免慢性發炎。
5. 做檢查、早發現:
定期健康檢查,有助於早期發現和及時治療代謝症候群。
 代謝症候群預防 5 絕招:逆轉有機會!
代謝症候群預防 5 絕招:逆轉有機會!
代謝症候群看似常見,但潛在風險不容忽視。透過健康的生活方式和定期檢查,我們可以有效預防和改善代謝症候群。如果你發現自己有腰圍變大的趨勢,不妨及時尋求醫師或營養師的幫助。保持健康,從現在開始!
※ 番外篇:想了解自己是否有骨質疏鬆、肌少症或肥胖症等問題?

每個人的天生體質、飲食習慣還有體態目標都不一樣,尋求醫生和營養師的協助,評估個人狀況,再規劃飲食內容,才能在不對身體造成傷害的狀況下,健康瘦下來!如果你有需要醫師與營養師為你規劃減脂/減重的計劃,歡迎預約許芷瑜醫師的控糖減肥門診,為你進行胰島素阻抗嚴重度評估、脂肪肝超音波減查、個人生理數值包含體重、體脂、肌肉量、內臟脂肪等重要指標的檢測,並指導你的個人化飲食。
前往預約
參考資料
國民健康署2017-2020年國民營養健康調查
Reaven G. M. (2001). Syndrome x: a short history. Ochsner journal, 3(3), 124–125.
國民健康署代謝症候群學習手冊
Stegemann, R., & Buchner, D. A. (2015). Transgenerational inheritance of metabolic disease. Seminars in cell & developmental biology, 43, 131–140. https://doi.org/10.1016/j.semcdb.2015.04.007
Al-Qawasmeh R. H, Tayyem R. F. Dietary and Lifestyle Risk Factors and Metabolic Syndrome: Literature Review. Curr Res Nutr Food Sci 2018;6(3). doi : http://dx.doi.org/10.12944/CRNFSJ.6.3.03
Chomiuk T, Niezgoda N, Mamcarz A and Śliż D (2024) Physical activity in metabolic syndrome. Front. Physiol. 15:1365761. doi: 10.3389/fphys.2024.1365761
Allen, J., Sun, Y., & Woods, J. A. (2015). Exercise and the Regulation of Inflammatory Responses. Progress in molecular biology and translational science, 135, 337–354. https://doi.org/10.1016/bs.pmbts.2015.07.003
Mann, S., Beedie, C., & Jimenez, A. (2014). Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: review, synthesis and recommendations. Sports medicine (Auckland, N.Z.), 44(2), 211–221. https://doi.org/10.1007/s40279-013-0110-5
Stebbings, G. K., Morse, C. I., McMahon, G. E., & Onambele, G. L. (2013). Resting arterial diameter and blood flow changes with resistance training and detraining in healthy young individuals. Journal of athletic training, 48(2), 209–219. https://doi.org/10.4085/1062-6050-48.1.17
Chomiuk T, Niezgoda N, Mamcarz A and Śliż D (2024) Physical activity in metabolic syndrome. Front. Physiol. 15:1365761. doi: 10.3389/fphys.2024.1365761
Gallardo-Alfaro, L., Bibiloni, M. D. M., Mascaró, C. M., Montemayor, S., Ruiz-Canela, M., Salas-Salvadó, J., Corella, D., Fitó, M., Romaguera, D., Vioque, J., Alonso-Gómez, Á. M., Wärnberg, J., Martínez, J. A., Serra-Majem, L., Estruch, R., Fernández-García, J. C., Lapetra, J., Pintó, X., García Ríos, A., Bueno-Cavanillas, A., … Tur, J. A. (2020). Leisure-Time Physical Activity, Sedentary Behaviour and Diet Quality are Associated with Metabolic Syndrome Severity: The PREDIMED-Plus Study. Nutrients, 12(4), 1013. https://doi.org/10.3390/nu12041013
Tristan Asensi, M., Napoletano, A., Sofi, F., & Dinu, M. (2023). Low-Grade Inflammation and Ultra-Processed Foods Consumption: A Review. Nutrients, 15(6), 1546. https://doi.org/10.3390/nu15061546
DiNicolantonio, J. J., & O'Keefe, J. H. (2018). Importance of maintaining a low omega-6/omega-3 ratio for reducing inflammation. Open heart, 5(2), e000946. https://doi.org/10.1136/openhrt-2018-000946
Dinu M, Tristan Asensi M, Pagliai G, Lotti S, Martini D, Colombini B, Sofi F. Consumption of Ultra-Processed Foods Is Inversely Associated with Adherence to the Mediterranean Diet: A Cross-Sectional Study. Nutrients. 2022; 14(10):2073. https://doi.org/10.3390/nu14102073
Canhada, S. L., Vigo, Á., Luft, V. C., Levy, R. B., Alvim Matos, S. M., Del Carmen Molina, M., Giatti, L., Barreto, S., Duncan, B. B., & Schmidt, M. I. (2023). Ultra-Processed Food Consumption and Increased Risk of Metabolic Syndrome in Adults: The ELSA-Brasil. Diabetes care, 46(2), 369–376. https://doi.org/10.2337/dc22-1505
Hosseinpour-Niazi, S., Bakhshi, B., Mirmiran, P. et al. Effect of weight change on the association between overall and source of carbohydrate intake and risk of metabolic syndrome: Tehran lipid and glucose study. Nutr Metab (Lond) 20, 39 (2023). https://doi.org/10.1186/s12986-023-00761-0
Cho, Y. A., & Choi, J. H. (2021). Association between Carbohydrate Intake and the Prevalence of Metabolic Syndrome in Korean Women. Nutrients, 13(9), 3098. https://doi.org/10.3390/nu13093098
Chandel N. S. (2021). Carbohydrate Metabolism. Cold Spring Harbor perspectives in biology, 13(1), a040568. https://doi.org/10.1101/cshperspect.a040568
NAKANISHI, Noriyuki, et al. “Cigarette smoking and the risk of the metabolic syndrome in middle-aged Japanese male office workers.” Industrial Health, vol. 43, no. 2, 2005, pp. 295–301, https://doi.org/10.2486/indhealth.43.295.
Balhara Y. P. (2012). Tobacco and metabolic syndrome. Indian journal of endocrinology and metabolism, 16(1), 81–87. https://doi.org/10.4103/2230-8210.91197
Baik, Inkyung, and Chol Shin. “Prospective study of alcohol consumption and metabolic syndrome.” The American Journal of Clinical Nutrition, vol. 87, no. 5, May 2008, pp. 1455–1463, https://doi.org/10.1093/ajcn/87.5.1455.
Wang, H. J., Zakhari, S., & Jung, M. K. (2010). Alcohol, inflammation, and gut-liver-brain interactions in tissue damage and disease development. World journal of gastroenterology, 16(11), 1304–1313. https://doi.org/10.3748/wjg.v16.i11.1304
Jurgens, Savana M., et al. “Inflammatory biomarkers link perceived stress with metabolic dysregulation.” Brain, Behavior, & Immunity - Health, vol. 34, Dec. 2023, p. 100696, https://doi.org/10.1016/j.bbih.2023.100696.
「一直發胖可能是這問題惹的禍?3大代謝警訊揭露糖尿病風險暴增6倍!|初日診所許芷瑜醫師【TODAY健面聊】」影片線上看
初日醫學
聯絡方式
地址|台北市中山區民生東路二段163號4樓
時間|週一至週五 10:00 - 18:00